It’s been a little over 5 years since my husband was first diagnosed with PTSD.
In those 5 years, I’ve seen, done and felt far too many things that a normal person should never have to see, do or feel in the context of marriage.
I’ve seen my husband on the verge of committing suicide. I’ve seen his physically violent outbursts where he randomly punches the wall, hurl objects at the wall and occasionally comes charging at me with hatred in his eyes.
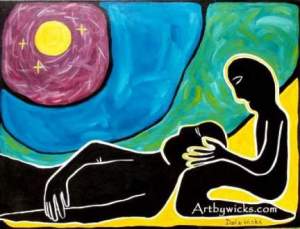
I’ve spent many years trying to block these images from flashing in my mind every now and then. Many nights I’ve lain awake beside him in fear of what else is to come. Some days I worry about my capacity to be emotionally strong for him when he needs an emotional anchor to get him through his worst times.
In the course of all these years, much as I try to remember to take care of myself, I forget to.
A couple of months ago I visited my therapist again. Her perspective states that the only thing I have to do is take time to take care of myself.
The best advice I ever got was talking not to my therapist… but to my husband’s therapist instead.
He has the benefit of perspective and knowledge about my husband’s condition and progress. He is familiar with the symptoms and specific manifestations of my husband’s condition. He is aware of what elements or events will trigger another attack. And he knows how I should deal with it when the time comes.
—
The therapist says my husband is definitely getting much better. The irony is that at this point in time, the lines between his condition and his true personality are starting to blur.
His insecurities about himself is a function of both his condition, his upbringing and in part because of his own personality.
His outbursts are manifestations of his personality, sadly just magnified by his condition.
His neediness and being clingy are manifestations of his insecurity.
He advises me on several things that had I known from the start, it would’ve helped me a great deal.
—
First. He needs to learn to stand on his own without me always there beside him.
I don’t always have to be there when he has his attacks or his flashbacks. He needs to learn to manage his own fears and his own attacks. Me being always there is not helping either of us.
Second. If I can’t handle it anymore, it’s better for me to stay away than be there and exacerbate his flashbacks or his latest uncontrollable emotional outbursts.
It’s counterproductive for both of us if I’m around but not in the condition to help him emotionally. So if I find myself in the middle of a situation where I’m tired and drained and unable to take what he’s dishing out — just leave the situation for awhile.
Third. It’s not about making all the emotions he feels disappear. It’s about learning to deal with them when they come.
The thing about PTSD is that it will always be there. There is no permanent cure. It will come, and it will go. The emotions and memories will always be a part of him… and therefore by default, will always somehow be a part of our marriage. The best thing at this point is to accept this fact, and together find a way to deal with it so it doesn’t get in the way of our marriage.
Fourth. Take time to be alone. As regularly as possible.
Both therapists actually advise me to take a few hours off every week just to take care of myself. Work doesn’t count. A few hours a week with no guilt to do whatever it takes to make me feel better and remind myself that I too matter, I too, have a life.
Fifth. Learn to disassociate.
The therapist also says: it is possible to deal with his outbursts and emotions without my own emotions getting in the way. However this happens, I have yet to learn it.
—
It continues to be a journey and a struggle today. There are good days, and there are bad days.
I have to admit. In the recent past, the thought of leaving him has entered my mind so many times. Somehow and some way though, I’m still around. I often wonder how much more of this I can take. I worry every time there’s a new attack, or a new episode if the next time around will be the last.
I don’t know what strength is in me that makes me keep enduring and championing on. I can’t deny how much I love him. But I also know love is not enough. And yet I’m still around. The foolish optimist in me keeps hoping that there will come a day that it will all be much better someday.